A team of Rice University engineers has launched a first-of-its-kind, open-source software that constructs and uses personalized computer models of how individual patients move to optimize treatments for neurologic and orthopedic mobility impairments.
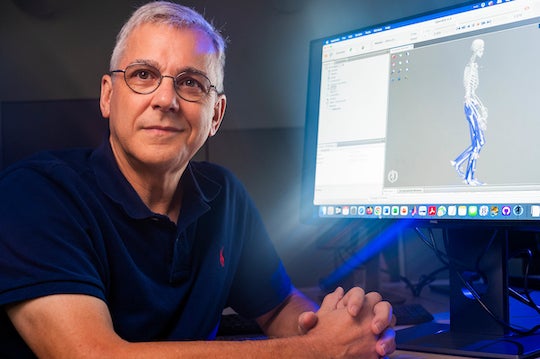
Funded by a grant from the National Institutes of Health, the Neuromusculoskeletal Modeling (NMSM) Pipeline software developed by B.J. Fregly and collaborators in the Rice Computational Neuromechanics Lab is now available to clinician/engineer teams that would like to utilize computer-aided engineering for clinical treatment design.
The software could be used to design orthopedic surgical plans, neurorehabilitation interventions, physical therapy regimens and prosthetic devices that maximize recovery of lost function for patients with movement impairments caused by stroke, osteoarthritis, cerebral palsy, Parkinson’s disease, spinal cord injury, traumatic brain injury, limb amputation and even some forms of cancer.
“Computer-aided engineering (CAE) software revolutionized the design of airplanes, automobiles and industrial equipment in the 1990s,” said Fregly, a professor of mechanical engineering and bioengineering and CPRIT Scholar in Cancer Research. “When I worked as a CAE software developer in industry during that time period, I kept thinking, someone needs to do this for the design of treatments for movement impairments.”
Many years in the making, the NMSM Pipeline builds upon existing software used to model, simulate and analyze the musculoskeletal system by making it useful for clinical treatment design.
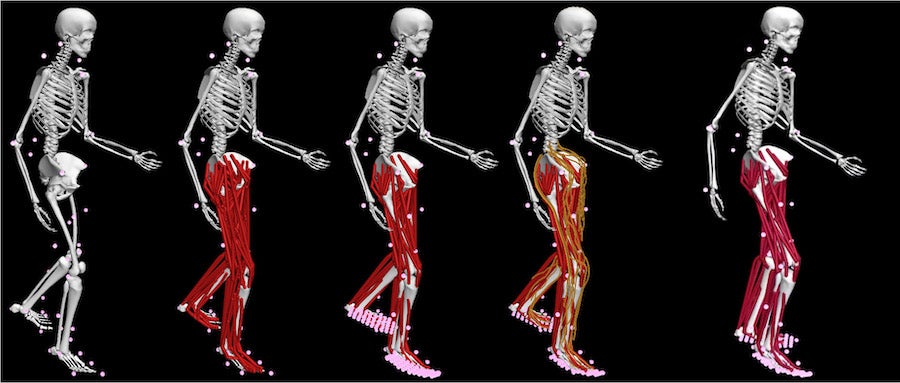
“Our software makes it easy to create a personalized computer model of a patient’s neuromusculoskeletal system using the patient’s pretreatment movement data, and it then uses that model to predict ⎯ and even optimize ⎯ the patient’s functional outcome for various treatment designs that a clinician wants to explore,” Fregly said. “For clinical utility, you need these two things ⎯ model personalization and treatment optimization.
“Instead of relying on implicit, subjective predictions of a patient’s post-treatment function, clinicians working with engineers could use our software to make explicit, objective predictions, which could not only weed out ineffective or harmful treatments, but also generate highly effective unforeseen ones.”
Click here to read the full article by Silvia Cernea Clark, Office of Public Affairs.